If you’ve been following Leqembi for Alzheimer’s (Leqembi is the brand name for generic lecanemab), you’ve probably noticed a gap between the headlines (“first disease-modifying therapy”) and real life (few people actually getting prescriptions.).
A major new Nature paper helps explain why that gap may not last. It suggests that when doctors are given clear eligibility criteria, structured imaging pathways, and manageable safety protocols, many more patients qualify than previously assumed. The result is not merely higher interest in Leqembi, but a realistic scenario in which prescriptions, not just discussions, could rise sharply. (Article continues below video…)
Researchers tested 11,486 community-dwelling adults in Norway using a highly accurate blood biomarker for Alzheimer’s pathology (plasma p-tau217)—a practical stand-in for the amyloid/tau changes that define Alzheimer’s disease neuropathological changes (ADNC). In other words, they measured the biology of Alzheimer’s at population scale, not just in memory clinics.
Their results imply that the “treatable” pool is far larger than current systems are built to handle—and that demand for drugs like Leqembi could rise sharply as blood tests become routine and eligibility is clarified.
What the study found (the numbers that change the story)
In participants 70 and older, the researchers estimated:
- 10% had preclinical Alzheimer’s (biological changes, but cognitively unimpaired)
- 10.4% had prodromal Alzheimer’s (often aligning with MCI)
- 9.8% had Alzheimer’s dementia
- Overall, ADNC positivity rose steeply with age—reaching 65.2% in those over 90.
- In the 70+ group overall, about 33.4% were ADNC-positive by their p-tau217 “rule-in” cut-off.
Most importantly for Leqembi planning: using contemporary treatment-eligibility logic (an algorithm based on current monoclonal antibody recommendations), 909 out of 8,949 people aged 70+—about 10.1%—met eligibility criteria for disease-modifying therapy.
That single number is the “demand multiplier.” It suggests a future where roughly one in ten older adults could be candidates—if the diagnostic pipeline is fast, standardized, and accessible.
- Preclinical AD: 10.0%
- Prodromal AD: 10.4%
- AD dementia: 9.8%
- AD pathology present in: 60% of dementia, 32.6% of MCI, 23.5% cognitively unimpaired
Where Leqembi is today: the uptake reality
It’s amazing to imagine that one in ten older adults could realistically be Leqembi candidates in the future. Now compare that to current use.
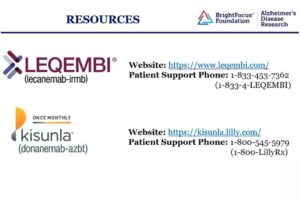
As of a company-cited update reported in early 2025, there were around 13,500 patients on Leqembi, with about 3,000 prescribers and 1,200 purchasing institutions in the U.S.
Even allowing for growth since then, this is still tiny relative to the likely eligible population.
The “now vs. where it could go” math (U.S. perspective)
A widely cited U.S. health-technology assessment (ICER) estimated about 1.4 million people in the U.S. could be eligible for anti-amyloid treatment in the early Alzheimer’s window.
Using the 13,500 treated figure as a concrete anchor:
- Estimated treated today: ~13,500
- Estimated eligible pool: ~1,400,000
- Share of eligible currently treated: ~0.96% (13,500 ÷ 1,400,000)
In other words: well under 1% of an estimated eligible pool—suggesting a 100x+ runway if infrastructure, referrals, and testing normalize.
The Nature study’s “~10% of 70+ eligible” result is directionally consistent with that kind of scale—especially once blood testing reduces friction and more people are diagnosed earlier.
Why this is caregiver-newsworthy (even if your family never uses Leqembi)
This study isn’t a “Leqembi works” paper. It’s a capacity and demand paper—and that matters to caregivers because it impacts:

- Wait times for neurology and memory clinics
- Access to confirmatory testing (PET scans, lumbar puncture, and now blood tests)
- Infusion capacity and MRI scheduling (ARIA monitoring)
- Insurance and payer rules as budgets collide with real-world prevalence
If health systems plan based on “tens of thousands,” but the biology suggests “hundreds of thousands to millions,” families may face longer queues—unless systems scale up proactively.
Practical takeaway for caregivers: what to do now
If your loved one has mild symptoms (or MCI) and you want to keep options open:
- Ask for a structured cognitive workup (not just “watchful waiting”).
- Discuss biomarker confirmation pathways (blood → PET/CSF, depending on location and coverage).
- Ask how MRI monitoring is handled if an antibody therapy becomes a consideration.
- Plan early for logistics: infusion site, transportation, caregiver availability, and follow-up MRIs.
Even if you decide “not for us,” the process of clarifying diagnosis earlier can improve planning, safety, and access to supportive resources.
The bottom line
This Nature paper is newsworthy because it suggests the Alzheimer’s “treatable pipeline” could be much larger than today’s treatment numbers imply—especially as scalable blood tests move from research into routine care.
If that happens, the limiting factor won’t be interest. It will be system capacity.
And that means: demand for Leqembi (and similar therapies) could look very different in the next few years than it does today.
How quickly Leqembi moves from approval to real-world use may shape Alzheimer’s care more than any single new therapy.