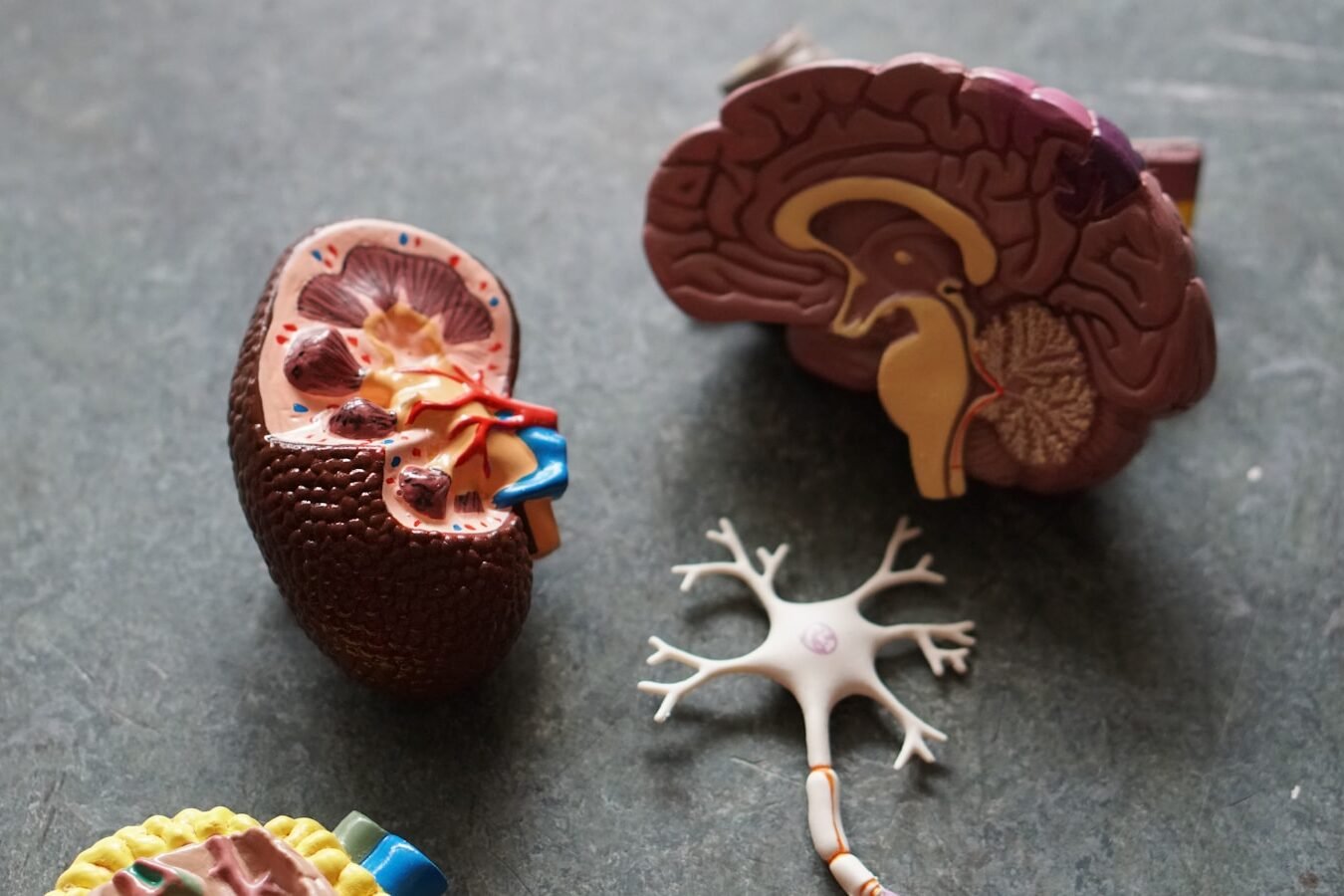
Alzheimer’s disease blood tests are becoming common tools for clinicians and researchers. But what if something outside the brain — like your kidneys — could influence those test results? A major new study suggests exactly that: reduced kidney function can elevate Alzheimer’s biomarkers in the blood without actually increasing someone’s overall risk of dementia. This matters for caregivers, families, and clinicians alike as we try to make sense of diagnostic data.
What the New Research Found
A study published in Neurology followed more than 2,200 adults (average age 72) for about eight years. Researchers tracked kidney function and levels of key Alzheimer’s-related biomarkers in the blood, including tau, amyloid beta, neurofilament light chain, and glial fibrillary acidic protein. They found:
- People with impaired kidneys tended to have higher blood levels of Alzheimer’s biomarkers, even when they were dementia-free.
- Poor kidney function did not increase overall risk of dementia compared to those with healthy kidney function.
- However, among people who already had elevated biomarkers, reduced kidney function appeared to accelerate dementia onset — especially in those with high neurofilament light chain levels.
These findings indicate that kidney health influences how biomarkers show up in the blood, but may not itself cause Alzheimer’s disease.
Why This Matters for Alzheimer’s Care
Amazon Books & Videos
about Alzheimer’s and Dementia:
FREE Newsletter:
Blood biomarkers are increasingly used to assess Alzheimer’s risk or progression. But if the kidneys are less effective at clearing proteins from the bloodstream, those biomarkers can accumulate and create a misleading picture. Other research confirms that even mild kidney dysfunction can elevate blood biomarkers and reduce the accuracy of predictive tests like neurofilament light chain.
For caregivers, this underscores a key point: test results should be interpreted in context. An elevated biomarker reading does not always mean more Alzheimer’s pathology — it could reflect reduced clearance due to kidney impairment.
More broadly, these findings highlight how interconnected organ systems are. The brain and kidneys both help regulate protein levels and waste removal — when one system falters, it can ripple outward.
What Caregivers and Families Should Do
- Talk with clinicians about kidney function. If your loved one has elevated Alzheimer’s biomarkers, ask whether kidney tests (like estimated glomerular filtration rate, eGFR) have been reviewed as part of the interpretation.
- Monitor kidney health proactively. Kidney function often declines subtly with age and with common conditions like hypertension and diabetes. Routine screenings can catch early dysfunction that could influence Alzheimer’s biomarker interpretation.
- Contextualize biomarker results. Biomarker levels are pieces of the puzzle — not diagnoses on their own. A comprehensive view that includes cognitive testing, clinical history, and organ health provides the most accurate perspective on Alzheimer’s risk.
Bottom Line
Emerging evidence shows that kidney health can affect Alzheimer’s biomarker levels in the blood, potentially confounding test interpretation. While poor kidney function doesn’t necessarily increase dementia risk, it may help explain why some people show elevated biomarkers. Caregivers and clinicians should consider kidney function when evaluating Alzheimer’s biomarkers and use that information as part of a broader clinical picture.