Early-evening restlessness and agitation, known as ‘sundowning’, is common in Alzheimer’s. So is fragmented sleep. A major discovery indicates these symptoms are curable.
People with Alzheimer’s often have poor biological rhythms, something that is a burden for both patients and their carers. Periods of sleep become shorter and more fragmented, resulting in periods of wakefulness at night and snoozing during the day. They can also become restless and agitated in the late afternoon and early evening, something known as ‘sundowning’.
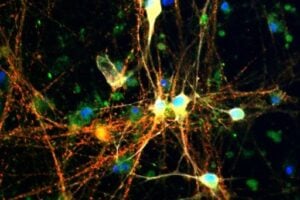
Credit: Dr. Stanislav Ott, Department of Genetics, University of Cambridge
Now, scientists from Cambridge have discovered that in fruit flies with Alzheimer’s the biological clock is still ticking but has become uncoupled from the sleep-wake cycle it usually regulates. The findings — published in Disease Models & Mechanisms — could help develop more effective ways to improve sleep patterns in people with the disease.
Biological clocks go hand in hand with life, and are found in everything from single celled organisms to fruit flies and humans. They are vital because they allow organisms to synchronise their biology to the day-night changes in their environments.
Until now, however, it has been unclear how Alzheimer’s disrupts the biological clock. According to Dr Damian Crowther of Cambridge’s Department of Genetics, one of the study’s authors: “We wanted to know whether people with Alzheimer’s disease have a poor behavioural rhythm because they have a clock that’s stopped ticking or they have stopped responding to the clock.”
The team worked with fruit flies — a key species for studying Alzheimer’s. Evidence suggests that the A-beta peptide, a protein, is behind at least the initial stages of the disease in humans. This has been replicated in fruit flies by introducing the human gene that produces this peptide.
Taking a group of healthy flies and a group with this feature of Alzheimer’s, the researchers studied sleep-wake patterns in the flies, and how well their biological clocks were working.
They measured sleep-wake patterns by fitting a small infrared beam, similar to movement sensors in burglar alarms, to the glass tubes housing the flies. When the flies were awake and moving, they broke the beam and these breaks in the beam were counted and recorded.
To study the flies’ biological clocks, the researchers attached the protein luciferase — an enzyme that emits light — to one of the proteins that forms part of the biological clock. Levels of the protein rise and fall during the night and day, and the glowing protein provided a way of tracing the flies’ internal clock.
“This lets us see the brain glowing brighter at night and less during the day, and that’s the biological clock shown as a glowing brain. It’s beautiful to be able to study first hand in the same organism the molecular working of the clock and the corresponding behaviours,” Dr Crowther said.
They found that healthy flies were active during the day and slept at night, whereas those with Alzheimer’s sleep and wake randomly. Crucially, however, the diurnal patterns of the luciferase-tagged protein were the same in both healthy and diseased flies, showing that the biological clock still ticks in flies with Alzheimer’s.
“Until now, the prevailing view was that Alzheimer’s destroyed the biological clock,” said Crowther.
“What we have shown in flies with Alzheimer’s is that the clock is still ticking but is being ignored by other parts of the brain and body that govern behaviour. If we can understand this, it could help us develop new therapies to tackle sleep disturbances in people with Alzheimer’s.”
Dr Simon Ridley, Head of Research at Alzheimer’s Research UK, who helped to fund the study, said: “Understanding the biology behind distressing symptoms like sleep problems is important to guide the development of new approaches to manage or treat them. This study sheds more light on the how features of Alzheimer’s can affect the molecular mechanisms controlling sleep-wake cycles in flies.
“We hope these results can guide further studies in people to ensure that progress is made for the half a million people in the UK with the disease.”
Source:
Journal Reference:
- K.-F. Chen, B. Possidente, D. A. Lomas, D. C. Crowther. The central molecular clock is robust in the face of behavioural arrhythmia in a Drosophila model of Alzheimer’s disease. Disease Models & Mechanisms, 2014; DOI:10.1242/dmm.014134












I have been taking care of my mother from dementia for 4 years I found this is really a very useful article for people who have dementia. thank you for sharing such a great article with us.
I read an article) about a care facility that comes alive late afternoon it has a. Their major activities start later in the day .If able to be outside they have lots of patio lights, dinner. Music a lot going on during those hrs
One such program is called, "Dusk 'Til Dawn." Enjoy this video that shows what it is all about:
Sundowning Care from Sunset 'til Sunrise
I care for my mother with severe dementia for 5 years now. When I first started living with here she had sun downing. I have since bought her a S.A.D. Lamp. And she has not have any sun downing since.
DO NOT USE PHRASES LIKE "…these symptoms are curable." I have Alzheimer's and so many media outlets use "hooks" like that to get clicks. This media outlet is now on my "Fake News list". I am adding a page to my website listing fake news sites like yours. Go to http://www.withalzmyheart.com to fing good links.
CARNOSINE PROTECTION AGAINST CIRCADIAN DISORDERS CAUSED BY "JETLAG".CARNOSINE is a well known support therapy in small doses (only under physician prescription) as a neuroprotector ,working as a peroxinitrites scavenger,antiglycating , mild heavy metal chelator ,lowers betamyloid accumulation,etc. In the article with the title : " The Effect of L-CARNOSINE on the Circadian Resetting of Clock Genes in the Heart of Rats" , by the authors Wu T. and colleagues, published in the journal Molecular Biology Reports (January 2015),we can read:"It is reported that the CIRCADIAN TIMING SYSTEM may be included in the mechanism by which L-CARNOSINE "PROTECTS" against multiple physiological alterations including blood glucose, cardiovascular functions etc. To clarify these issues, the authors compared the EFFECTS of CARNOSINE ON THE EXPRESSION OF CIRCADIAN GENES IN THE HEART OF RATS UNDER CONTROL AND JET LAG CONDITIONS. CARNOSINE FEEDING OBVIOUSLY ENHANCED THE RESETTING RATES OF CLOCK GENES in the heart of normal rats after the experimental JET LAG.CARNOSINE FEEDING PLAYS A POSITIVE ROLE IN THE CIRCADIAN RESYNCHRONIZATION OF THE HEART CLOCK"
Anecdotally speaking, it makes sense that the biological clock (very primitive brain function) is still intact in Alzheimer's disease, but the poorer functioning higher level cognitive functions override the impulse to sleep. Chronic anxiety and overthinking cause most of us to wake up during the night. We all demonstrate that behavior at some point, and regardless of how tired we are, troubling thoughts or underlying agitation disrupt our sleep patterns. And how do we deal with feelings of unrest or anxiety? We move. We wring our hands, we pace, we clean- we try to work through our issues through movement. Maybe some of us talk it out or write down our thoughts to clear our minds, but language is frequently impaired in Alzheimer's which is yet another source of anxiety for the person. So as far as actual solutions go, either we reduce the activity in the overactive brain through meds or distraction, or we increase the movement opportunities while awake.
I understand those that were disappointed by the 'no cure' only reason information contained in the article. But I believe the point was that, now that we know it's not the Alzheimer's that is creating the disruption in their brain regarding time of day and sundowning, we can at least look for a cure or solution to help with the disruption. That the disruption is not futile.
As for practical solutions to the caregiver's problems (my heartfelt sympathy, Jessica!) … you cannot treat the symptoms effectively without determining what might be causing them. The articles I cited, on sleep disturbances and "sundowning", discuss the various possible causes and some potential solutions. And I fervently hope you figure out what works for your loved one!
http://www.alzcompend.info/?p=214
http://www.alzcompend.info/?p=268
I ended up having to think WAY outside the box, and asked my husband's doctor if we could try prazosin. She was knowledgeable about its use in treating PTSD and the clinical trials for treating agitation in Alzheimer's patients, and prescribed it for him.
Blessed sleep!
My husband was getting depressed without me realising it. When the doctor took him off sleeping pills of any kind and we replaced these with anti-depressant pills his mood lifted and he is really on top form. The sleeping disturbances still happen at night, related in part to my mood, where I am in the house and his anxieties. I have night Carers to take over some nights so I get a full night's reat. He has adjusted to this and we continue to live together at home – a home from Home. The day he goes into a Home is when he knows me/us no more at all.
Lilian, I am also keeping my husband home with me as his main care giver and he does have some sun downing causing his to become agitated. I think my husband is more bored than depressed. What agitates me the most is almost all of my friends just keeping asking me when I am putting him in a home. Do have this issue also?
I agree with Jackiemartinart, for a number of reasons.
(1) Dementia patients often suffer from sleep disturbances. However, they can be caused by many different factors, including not only medications, but also pain (e.g., arthritis, muscle aches, dental problems, untreated ear or sinus infections, or a urinary tract infection); physical discomfort from e.g., bladder or incontinence problems, enlarged prostate, etc; a sleep disorder such as restless leg syndrome, REM sleep behavior disorder, nocturnal myoclonus, or sleep apnea, which are relatively common in elderly individuals and/or may be a result of the disorder causing the dementia; and/or depression. See:
http://www.alzcompend.info/?p=214
(2) The term "sundowning" is, at best, a misnomer. Broadly speaking, sundowning is a cyclical increase in agitation (which may include restlessness, confusion, disorientation, wandering, searching, escape behaviors, tapping or banging, vocalization, combativeness, and/or hallucinations) that takes place at roughly the same time every day. Despite its name, and the wide-spread belief that sundowning occurs in the late afternoon and early evening, studies have found that the peak of sundowning activity is just as likely to occur in the early morning for a given individual, or in the early- to mid-afternoon (e.g., around 1:00pm), while in some patients, it may occur late at night. Sundowning and sleep disturbance may appear to be related to each other since a sleep disorder, such as sleep disordered breathing, can be associated with daytime behavior disorder.
There is a popular hypothesis that sundowning is a chronobiological phenomenon that is unrelated to sleep disturbances but, rather, by a disturbance in the normal circadian rhythms. Results of studies on this hypothesis, and potential related treatments such as bright light therapy and/or melatonin supplements, have produced conflicting and contradictory results, however. Moreover, the roles of melatonin and its associated receptors and the effects of Alzheimer's on their expression are very complex and not at all well-understood.
Some studies have concluded there is no such thing as sundowning per se.
See:
http://www.alzcompend.info/?p=268
To continue:
(3) While the fruit fly study is interesting and quite elegant, it is quite a stretch to draw conclusions about dementia patients from studies on genetically engineered Drosophila.
Organisms ranging from bacteria to humans exhibit daily (circadian) rhythms. In fact, circadian rhythms are found in individual cells, tissues, and organs as well as in the overall "whole" organism. Several lines of evidence point to the fact that the transcription and translation of genes, or even the presence of DNA in the cell, are not necessary for the circadian rhythms to occur. See:
http://blogs.scientificamerican.com/observations/2011/02/11/circadian-clock-without-dna-history-and-the-power-of-metaphor/
This article says that "A-beta peptide, a protein, is behind at least the initial stages of the disease in humans. This has been replicated in fruit flies by introducing the human gene that produces this peptide." Well … no. In the human brain, the transmembrane protein, amyloid precursor protein (APP), is produced. A-beta peptides, either a 40- or 42-amino acid chain, are produced by the proteolytic cleavage of APP by beta- and gamma-secretases. Lipid rafts are involved in the regulation of APP proteolytic processing and A-beta generation, and it is thought that the aberrant lipid content of the neuron membranes in the Alzheimer's brain causes improper APP cleavage that leads to the formation of Alzheimer's plaque.
The fruit flies in the study do not replicate the proteolytic processing of APP. Instead, the researchers have "fused the A-beta peptide with a secretion signal peptide and driven its expression in the nervous system." I.e., instead of A-beta 1-40 or A-beta 1-42 being produced, the fruit flies produce a chimeric polypeptide that, by definition, has a structure far different from Alzheimer's A-beta, and unknown functions/properties in the fruit fly nervous system.
Lovely article…but it gives no hope for the caregiver. The body needs rest…when loved ones don't sleep neither does the caregiver….how about publishing an article with applied knowledge pertaining to actual solutions.
Dear Jessica
I guess that a medicine doctor especialized in neuropsychiatry, with experience with dementia patients,maybe can prescribes small doses of some drugs that can help the dementia patient to sleeps (but only under physician prescription and giving the lowest dose
(as a dose for a small child) and controlling blood presure).
Talk to the doctor about it.
Well put, Jessica. I get all excited when I see a headline, such as the one that pulled me into reading this article, only to learn that there isn't anything available right now. Working in a 30 bed assisted living facility for memory care residents, we are dealing with several individuals who have been admitted because their family caregiver just wore out trying to keep up with someone sundowning and awake all night. Current options include sleeping pills or antipsychotics, which we DO NOT use because of the increased risks involved. Our saving grace is that we have a night shift who remain awake and on duty, often following, attempting to redirect, and always striving to keep said residents safe. But for those who still have their loved ones at home, I find it misleading to read articles such as this.
You're certainly touching an essential need for "applied knowledge pertaining to actual solutions" There are articles and videos about it on this site. Just go to the right hand column, find the box with the title "Pick a Topic" and click on "SUNDOWNING".
Judy, I think that most facilities need to change their routine to fit the patients needs (vs medicating). I stumbled upon an article about a program run at a facility in NYC. They have a dedicated team from 7 pm to 7 am that run an activity program for those who are up all night. We often try to change the individuals normal body cycles to fit the 'regular' world. I am a caregiver to my Mom (age 91) ….. she was always a night owl and I rise at dawn ! I now have altered my schedule to fit hers ( I go back to bed for a while or catch a nap if someone can cover for me). This works ! Mom is no longer on sleep medication which produced it's own nasty after effects. I wish more care facilities would use logical thinking when trying to solve problems . In most situations in life if something is not working we figure out a better plan. I don't know why this isn't obvious in this situation !
To see the "After-Sundown" program discussed in the previous posts, click on:
Sundowning Solution: Care from Dusk 'Til Dawn
Jessica, the psychiatrist prescribed quetapel for my husband and since taking the medication we sleep through the night, first time in years.
I agree with the comment that these sorts of articles are very interesting but don't give any hope or help to the caregiver. I am so tired of reading "Try distracting them." My mother has memory and attention problems, so she is distracted all the time. We have tried changing routines, using different medications, checking for unarticulated pain, increasing physical and cognitive activities during the day, putting up curtains that can block out lights at night, you name it we have tried it. Melatonin supplements, eating before bed, not eating before bed, etc. Antipsychotics made it worse, although they improved cognition. Sedatives keep her sleepy but she still gets up and wanders all night. Better to publish the list of things people have actually tried that actually work.
I dont believe sundowning and disrupted sleep are necessarily related and should be looked on as separate issues. Working in a nursing home, once the light starts to fade, the anxiety levels rise and the wandering starts. The mind goes back to how they normally would have ended their day, finishing work, get home, get the dinner on etc. Disrupted sleep is often medication related
Thank you for your interpretation of sundowning and sleep-related behaviour. Less light means that my husband sees less well and becomes quite confused and disorientated, even at home. Out and about his anxiety gets worse at sundown / dusk, as if he is searching for appropriate behaviour but cannot find any memories to draw on to support him. He needs an enormous amount of reassurance at sundown/dusk, and then he will trust and follow my lead. I agree sleep-related disturbances are partly caused by medication imbalances. My husband's chronological clock has been disrupted by brain damage, so he needs reminding about what time it is, and he rarely associates the coming and going of daylight with set behaviours – he has forgotten / lost a lot of the memories we take for granted. I really believe that everyone is unique in their behaviour, but some generalities can also really help the Carer decide how to respond for the best. Thank you again.
While I respect that you work with patients daily I can assure you the issues are correlated. I am with my mother 24/7 and I shift my sleep to mimic hers to protect her from hurting herself, I have found that exercise does help as well as maintaining a balanced diet. We eat as little processed foods as possible, fresh is best but I also include coconut oil and see huge benefits that have been confirmed over the last 6 years when my cooking habits change or I don't include it in her food ( our since we eat the same foods) daily and when I get her back on it cognitive acuteness improves almost immediately ( it takes time at first but re-introducing it is immediate) and there needs to be more progress on the immediate energy given the brain from the coconut oil and how it helps with even sundowning
My husband sleeps til almost noon everyday. When we have an appointment, it's all I can do to arouse him and get him to shave and dress himself to leave after breakfast. Then he has forgotten where we are going and who we're going to see. He absolutely refused to come into the office waiting room today and I had to convince him that he just had to wait for me and then he sat and read a magazine. As for sleeping at night, he's good at falling asleep just after the news and as I said before sleep until almost noon. He hasn't experienced 'sundownners' as yet. Maybe it's just him or another thing to 'look forward to'.
A wonderful study, thank you! As a professional in the field of dementia I had never considered the idea of certain parts of the brain ignoring the biological signal to sleep. Well done!