Alzheimer’s disease, long thought to be a single disease, really consists of three distinct subtypes, according to a UCLA study.
The finding could lead to more highly targeted research and, eventually, new treatments for the debilitating neurological disorder, which robs people of their memories.
The study further found that one of the three variations, the cortical subtype, appears to be fundamentally a different condition than the other two, said Dr. Dale Bredesen, the study’s author, a UCLA professor of neurology and member of the Easton Laboratory for Neurodegenerative Disease Research.
“Because the presentation varies from person to person, there has been suspicion for years that Alzheimer’s represents more than one illness,” said Bredesen, who also is the founding president of the Buck Institute for Research on Aging. “When laboratory tests go beyond the usual tests, we find these three distinct subtypes.
“The important implications of this are that the optimal treatment may be different for each group, there may be different causes, and, for future clinical trials, it may be helpful to study specific groups separately.”
3 Subtypes
The subtypes are:
- Inflammatory, in which markers such as C-reactive protein and serum albumin to globulin ratios are increased.
- Non-inflammatory, in which these markers are not increased but other metabolic abnormalities are present.
- Cortical, which affects relatively young individuals and appears more widely distributed across the brain than the other subtypes of Alzheimer’s. It typically does not seem to cause memory loss at first, but people with this subtype of the disease tend to lose language skills. It is often misdiagnosed, typically affects people who do not have an Alzheimer’s-related gene and is associated with a significant zinc deficiency.
The findings of the two-year study, which involved metabolic testing of 50 people, appear in the current issue of the peer-reviewed journal Aging.
No effective therapy for Alzheimer’s exists. And scientists have yet to completely identify the cause, although multiple studies have pointed to metabolic abnormalities such as insulin resistance, hormonal deficiencies and hyperhomocysteinemia, a condition characterized by an abnormally high level of an amino acid in the blood.
In an earlier paper, Bredesen showed that making lifestyle, exercise and diet changes designed to improve the body’s metabolism reversed cognitive decline in nine out of 10 patients with early Alzheimer’s disease or its precursors.
The current finding grew out of an extensive evaluation of the data from last year’s study, and it could eventually help scientists pinpoint more precise targets for treatments — the same approach that has led to major advances in treating other diseases.
For example, Bredesen explained, researchers have recently been able to develop precise treatments for cancer by sequencing tumor genomes and comparing them to the patients’ genomes to better understand what drives the formation and growth of tumors.
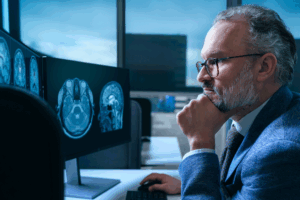
“However, in Alzheimer’s disease, there is no tumor to biopsy,” Bredesen said. “So how do we get an idea about what is driving the process? The approach we took was to use the underlying metabolic mechanisms of the disease process to guide the establishment of an extensive set of laboratory tests, such as fasting insulin, copper-to-zinc ratio and dozens of others.”
Advanced Categories: 6 Subtypes of Alzheimer’s
Dr. Bredesen subsequently designed a more refined subtyping of Alzheimer’s, with 6 subtypes. The 6 subtypes are as follows:
- Type 1 Alzheimer’s disease is inflammatory, or hot
- Ongoing or chronic inflammation puts you at greater risk for developing Alzheimer’s
- Type 2 Alzheimer’s disease is atrophic, or cold
- Sub-optimal levels of nutrients, hormones, trophic factors (cell growth factors like NCF, nerve growth factor) increases your risk for Alzheimer’s disease.
- Type 1.5 Alzheimer’s disease is glycotoxic, or sweet
- High blood sugar or high fasting insulin levels increase your risk for Alzheimer’s disease. It is termed Type 1.5 because it has features of both Type 1 and Type 2. High cholesterol may also come into play.
- Type 3 Alzheimer’s disease is toxic, or vile
- Exposure to toxins such as mercury, toluene, or mycotoxins (made by certain types of mold) leads to an increased risk for Alzheimer’s disease. Although we all experience this exposure to a greater or lesser degree, the key is to minimize it by identifying and removing or minimizing exposures.
- Type 4 Alzheimer’s disease is vascular, or pale
- If you have cardiovascular disease, you are at an increased risk of Alzheimer’s disease. Vascular leakiness is one of the earliest changes identified in Alzheimer’s disease.
- Type 5 Alzheimer’s disease is traumatic, or dazed
- A history of head trauma — from accidents, falls, or repeated sports-related head injuries — increases your risk for Alzheimer’s disease.
Most patients with Alzheimer’s disease have more than one type and present multiple risk factors.
Alzheimer’s Causes and Treatments
Going forward, Bredesen and his team will seek to determine whether the subtypes have different underlying causes, and whether they respond differently to potential treatments.
The need for a new approach to treat Alzheimer’s is urgent. It is the most common age-related dementia, and the number of people with the disease in the U.S. is expected to increase to 15 million in 2050, from nearly 6 million today. The cost to treat people in the U.S. with Alzheimer’s and other dementias is expected to be $226 billion in 2015 alone, and could reach $1.1 trillion in 2050.
- UCLA, University of California at Los Angeles