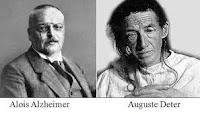
Older adults at greater risk of dementia may be able to decrease their risk of cognitive decline by nearly half by using hearing aids, according to a study published in The Lancet.
Dementia Books & Videos on Amazon:
FREE Newsletter:
Over a decade of research has established hearing loss as a major risk factor for dementia, but the study is the first randomized controlled trial to clarify whether intervening with hearing aids would diminish the risk. The WHO estimates that by 2050 over 700 million people—1 in 10—will have disabling hearing loss, so this research has major implications.
In this Q&A, adapted from the July 21 episode of Public Health On Call, Stephanie Desmon speaks with Frank Lin, MD, PhD ’08, lead author of the study and director of the Cochlear Center for Hearing and Public Health, about his findings and how they could improve the future of millions with hearing loss.
What can you tell us about your new study in The Lancet?
For over a decade, our research has increasingly been making a case for how hearing loss can impact dementia risk. Epidemiological studies over the last several years suggest that hearing loss may be the largest contributor to dementia out of all known risk factors.
The question then is: If we treat hearing loss in older adults, does that reduce cognitive decline as well as possible risk of dementia? That’s always been unknown, because there’s never been a randomized controlled trial until now.
Tell us more about that tria
In late 2017 we started this trial that involved nearly 1,000 older adults ages 70 to 84 recruited at four different field sites around the U.S. They each had mild to moderate level hearing loss, and they all had intact cognition and no substantial cognitive impairment.
We recruited from two different populations. At every site, there was a population of older adults who were already participating in the Atherosclerosis Risk In Communities (ARIC) study, which for the past 30 years has followed a random sample of older adults to monitor cardiovascular health. About a quarter of the sample came from the ARIC participants. The other three-quarters of the sample were healthy community volunteers who responded to advertisements about a healthy aging study.
When we started the study, we noticed that on average, the ARIC participants were slightly older than the healthy volunteers, and in general they had more risk factors for cognitive decline, such as higher levels of high blood pressure and diabetes and slightly lower education and income than the new healthy volunteers who came in.
At the beginning of the study, the participants were randomized into two groups. Half got best-practices hearing intervention: meeting with an audiologist over four sessions, getting hearing aids—everything to support their hearing communication needs. The other half got a health education control intervention: meeting with a health care educator to go over topics that are critical for healthy aging like nutrition, vaccinations, etc. Everyone had the same amount of exposure to study personnel.
Everyone was then followed for three years, with visits every six months during which their cognition was assessed with a standardized battery of thinking and memory tasks.
What we found was unanticipated, but the results make complete sense in hindsight. After three years, the rate of cognitive change was no different for the people who got the hearing intervention than people who got the control intervention. The story deepens though. When we looked at the groups separately, we saw something really different. ARIC participants who had the hearing intervention had half the rate of cognitive change over three years than people in the control group. In contrast, in the healthy volunteers, we saw the same rate of cognitive change as those who were in the control group, meaning the hearing intervention didn’t do much.
We think we saw a huge reduction in cognitive decline with the hearing intervention in the ARIC group because this group actually had cognitive decline, while the healthy community volunteers didn’t really have much cognitive change at all. It’s hard for a hearing intervention to slow something down that’s already really, really slow.
So, if a person has risk factors for cognitive decline other than being older, this hearing intervention could really help?
When people get hearing intervention, there’s always a theoretical possibility that it may support cognitive function over the long term. The more important thing to think about is the more proximal effects: Hearing intervention can definitely improve communication benefits and help you socially engage more.
The clinical takeaway is that almost anyone with hearing loss as an older adult should get their hearing checked and address hearing issues if there are any. There’s really no downside to it. Hearing intervention comes at no risk.
Can it help your cognition in the short term if you’re a completely cognitively healthy person? No, but it can help cognition in the longer term. That longer-term study for healthy people is what we’ll do over the next several years.
Are these results an argument for why Medicare should start covering over-the-counter hearing aids?
We certainly hope so. In this trial, hearing aids were one part of the hearing intervention. The other big part is the audiologist who’s there to help the person, support their use of devices, convince people that hearing aids can help them, show them how to use it, and customize it for their lifestyle. Not everyone needs that level of service, but for a lot of people in their 70s and 80s, who may not be as familiar with technology, those audiological support services are key.
OTC hearing aids come with a caveat. In the next year or two, we’re going to have phenomenal, much lower cost hearing aids on the market, but many people will still need the services of an audiologist to help them use those devices to their fullest.
The bitter irony is that the intervention we delivered would not be covered by insurance right now in the U.S. That’s something we hope to change. We need to ensure that the services seniors will need to benefit fully from hearing aids become available. We think reducing cognitive decline could in the longer term actually reduce rates of dementia, which is a really compelling “money-in-the-bank” financial argument for Medicare to cover.
What is the link between hearing loss and cognitive decline?
There are three major theories. The first is the idea that when you have hearing loss, you may not be as socially engaged. You may become more lonely or withdrawn. One thing we know about risk of dementia and cognitive decline is that if people don’t remain engaged with cognitively stimulating activities, it is not good for the brain.
Another theory is that when you have hearing loss, your brain is not getting a clear sound from your ear, and the brain compensates by constantly reallocating resources to help with hearing, at the expense of thinking and memory abilities or helping protect the brain against other pathology that can lead to dementia. In that situation, it’s not just that hearing loss causes dementia, but hearing loss taxes the brain and leads to earlier exposure dementia from other factors that can lead to dementia. That’s called a cognitive load hypothesis.
The third idea is that hearing loss can directly have negative effects on the brain’s structural integrity. With constant reduced auditory stimulation of parts of the brain, parts of the brain can begin atrophying faster. As you can imagine, a shrinking brain is not good for brain function.
All three theories suggest that treating hearing loss with something as simple as using a hearing aid could directly modify or affect those pathways and reduce the risk of cognitive decline.
The whole reason we treat hearing loss is to keep people engaged. From a proof-of-concept perspective, we think hearing aids and hearing treatment can make a difference. And that’s what we’re seeing right now with the results of this trial.
SOURCE:
Johns Hopkins Bloomberg School of Public Health
REFERENCE:
Lin FR, Pike JR, Albert MS, ArnoldM, Burgard S, Chisolm T, et al. Hearing intervention versus health education control to reduce cognitive decline in older adults with hearing loss in the USA (ACHIEVE): a multicentre, randomised controlled trial. The Lancet July 17, 2023. DOI: https://doi.org/10.1016/S0140-6736(23)01406-X









I have been reading articles for you guys for a little over a year, since my Dementia diagnosis (at age 59). I find it offensive and reckless for you the promote moronic studies that all claims to be a miracle cure for Dementia. It is very discouraging and I find it disgusting. It makes you guys look like people who don’t really understand or care about folks battling with Dementia, you give them false hope and likely make money in the process. SHAME!!
Not sure what upset you. There are no posts on this site that promote any cure for dementia, miracle or otherwise. In addition, this site only posts studies from internationally recognized and accredited institutions. I thought perhaps I was missing something, so I asked, “Anyone know what you’re referring to?” No one came up with anything. Excuse me for my lack of success in trying to help you, but could you tell me what you might be referring to?