Patients treated in intensive care units across the globe are entering their medical care with no evidence of cognitive impairment but oftentimes leaving with deficits similar to those seen in patients with traumatic brain injury (TBI) or mild Alzheimer’s disease (AD) that persists for at least a year, according to a Vanderbilt study published in the New England Journal of Medicine.
The study, led by members of Vanderbilt’s ICU Delirium and Cognitive Impairment Group, found that 74 percent of the 821 patients studied, all adults with respiratory failure, cardiogenic shock or septic shock, developed delirium while in the hospital, which the authors found is a predictor of a dementia-like brain disease even a year after discharge from the ICU.
Delirium, a form of acute brain dysfunction common during critical illness, has consistently been shown to be associated with higher mortality, but this large study of medical and surgical ICU patients demonstrates that it is associated with long-term cognitive impairment in ICU survivors as well.
At three months, 40 percent of patients in the study had global cognition scores similar to patients with moderate TBI, and 26 percent scored similar to patients with AD.
Deficits occurred in both older and younger patients, irrespective of whether they had coexisting illness, and persisted to 12 months, with 34 percent and 24 percent still having scores similar to TBI and AD patients, respectively.
“As medical care is improving, patients are surviving their critical illness more often, but if they are surviving their critical illness with disabling forms of cognitive impairment then that is something that we will have to be aware of because just surviving is no longer good enough,” said lead author Pratik Pandharipande, M.D., MSCI, professor of Anesthesiology and Critical Care.
“Regardless of why you come in to an ICU, you have to know that, on the back end of your critical care, you are very likely to be suffering cognitively in ways similar to a TBI patient or an AD patient, except that most of the medical profession doesn’t even know that this is happening and few around you suspect anything, leaving most to suffer in silence,” said senior author Wes Ely, M.D., professor of Medicine.
“Delirium in critically ill, hospitalized adults is a serious yet understudied issue,” said Molly Wagster, Ph.D., chief of the Behavioral & Systems Neuroscience Branch in the National Institute on Aging, part of the NIH. “These new findings provide important evidence of the extent of the problem, the imperative for greater recognition and the pressing need for solutions.”
Ely said at least some component of this brain injury may be preventable through efforts to shorten the duration of delirium in the ICU by using careful delirium monitoring and management techniques, including earlier attempts at weaning from sedatives and mobility protocols that can save lives and reduce disability.
“Even after the patient leaves the hospital, we think that cognitive rehabilitation might be helpful to somebody like this, and we have some early preliminary data supporting this,” he said.
MORE INFO:
This project was supported by grants from the National Institutes of Health (AG027472, AG035117, AG034257, AG031322, AG040157, HL111111, and 2 T32 HL087738-06), and the Veterans Affairs Tennessee Valley Geriatric Research, Education and Clinical Center and the VA Clinical Science Research and Development Service.
SOURCE:
Vanderbilt University Medical Center, via Newswise.
REFERENCE:
P.P. Pandharipande, T.D. Girard, J.C. Jackson, A. Morandi, J.L. Thompson, B.T. Pun, N.E. Brummel, C.G. Hughes, E.E. Vasilevskis, A.K. Shintani, K.G. Moons, S.K. Geevarghese, A. Canonico, R.O. Hopkins, G.R. Bernard, R.S. Dittus, E.W. Ely. Long-Term Cognitive Impairment after Critical Illness. New England Journal of Medicine, 2013; 369 (14): 1306 DOI: 10.1056/NEJMoa1301372




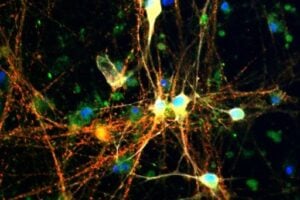






There are some articles that can works as a base for more research with that supplements for neuroprotection against delirium,cognitive impairments,and in cardiomyocytes protection after heart attacks:
1)Neuroprotection by acetyl l carnitine in traumatic brain injury.
“Traumatic Brain Injury(TBI)it is cause of mortality and morbidity in children and is characterized by reduced aerobic cerebral energy metabolism early after injury.Acetyl L carnitine is metabolized in the brain to acetyl coenzyme A.Acetyl Carnitine administration is neuroprotective in animal models of cerebral ischemia and spinal cord injury.Treatment with acetyl carnitine within the first 24 hours after TBI IMPROVES behavioral outcomes and REDUCES brain lesion volume in immature rats within the first 7 days after injury”.(Neuroprotection by acetyl-L-carnitine after traumatic injury to the immature rat brain. Scafidi S,USA.-Dev Neurosci. 2010)
2) Neuroprotection by Carnosine in stroke by right unilateral common carotid arteries occlusion in rats:
In summary:“ AFTER to right unilateral common carotid arteries occlusion in rats CARNOSINE protected against NMDA excitotoxicity, ameliorated white matter lesion,and reduced cognitive impairment, supressed the activation of microglia (controlling neuroinflammation) significantly ATTENUATED the increase in reactive oxygen species generation and largely REVERSED myelin basic protein decrease(atrophy)in the corpus callosum.(Protective Effect of Carnosine on Subcortical Ischemic Vascular Dementia in Mice.-Ma J-CNS Neurosci Ther. 2012)
3)Neuroprotection by Carnosine against anesthetic toxicity.
title of the article :Carnosine protects against the neurotoxic effects of a serotonin-derived melanoid:
In summary:“Anesthesia-related postoperative cognitive dysfunction leads to morbidity in the elderly.Lipid peroxidative byproducts(acrolein)accumulate in aging.Sevoflurane, an inhaled anesthetic, sequesters acrolein and enhances the formation of a serotonin-derived melanoid(SDM).Treatment with L-Carnosine PROTECTED differentiated brain cells exposed to SDM.Neuronal impairment is prevented by L-Carnosine.”(Carnosine protects against the neurotoxic effects of a serotonin-derived melanoid. Brownrigg TD published in:Neurochemistry Research.2011)
4)Synergistic effects in neuroprotection by the association of the acetyl-l-carnitine and n-acetyl-cysteine in peripheral nerve injury
Title of the article:“The nerve injury and the dying neurons: diagnosis and prevention.”:In summary:“Pharmacological intervention sing either Acetyl-L-CARNITINE or N-Acetyl-CYSTEINE give complete neuroprotection in different types of peripheral nerve injury"
“Both compounds are clinically safe and experimental work has defined the best dose,timing after injury and duration of administration.
The efficacy of neuroprotection of either supplements can be monitored non-invasively using MRI,as demonstrated experimentally and more recently by clinical studies of the volume of dorsal root ganglia”(The nerve injury and the dying neurons: diagnosis and prevention.Terenghi-J Hand Surg Eur Vol. 2011)
5)CARNOSINE IN HEART AND/OR BRAIN ISCHEMIA
Title of the article :ANTI-ISCHEMIC ACTIVITY OF CARNOSINE:
In summary:“This review summarizes the data on anti-ischemic activity of carnosine.The pronounced ANTI-ISCHEMIC effects of CARNOSINE in the BRAIN AND HEART are due to the combination of antioxidant and membrane-protecting activity, proton buffering capacity, formation of complexes with transition metals, and regulation of macrophage function.In the experiment,CARNOSINE decreases mortality and is beneficial for neurological conditions of the animals. In cardiac ischemia, carnosine protects cardiomyocytes from damage and improves contractility of the heart” (ANTI-ISCHEMIC ACTIVITY OF CARNOSINE.Authors Stvolinsky SL, et al.Journal Biochemistry,2000)
Maybe the research article above , can be used by medicine doctors that are specialists in neurosurgery, neurology, cardiology and doctors that works in ICU to find some support or augmentation therapy that can works not only in the vascular levels , but that can gives neuroprotection to the brain and heart muscle protection , in the molecular , biochemical ,metabolical levels , in cases like:
1) Patients that suffered a severe stroke or a heart attack :
The doctors treat with drugs and/or stents or surgery , to open the closed coronary heart artery in cases of heart attacks and of the neck and/or brain artery in cases of ischemic stroke, and gives ICU support, with oxygen, blood pressure drugs , etc., and the doctors do their best to treat the artery lesions, and other complications.
But in the cellular level, in the neuron cell level, what are the drugs or supplements that doctors can gives as a augmentation or support therapy to treat the metabolical, molecular and biochemical neuron cells and astrocytes disorders during the time that the patient was in the ICU , and after the patient go to his home with cognitive disorders ,and to gives the same cellular support to the heart muscle cells in cases of heart attacks?
2) In the same way, patients that had to be in the ICU by weeks or months, under induced or non induced coma , after the recovery , and after he is discharged to his home, what are the drugs or supplememts used to treat the neuron sequelaes of that disorders (as delirium, cognitive impairments,etc)?
When we do some search in scientific research sites , we can find a lot of drugs and supplements that could help that patients , during and after the hospital time, as smart drugs, as L-carnosine, taurine, acetyl L carnitine, vipocentine Citicoline (CDP-Choline) , glucaric acid,etc.
The studies about that drugs as strong neuroprotectors are in the sites as the medical scientific site called PubMed.
My father had some mild cognitive problems before going in for an aortic valve replacement with a pig valve. It took 3 days for him to wake up from the anesthesia and when he did he was a completely different person. His cognitive problems were so severe that he was diagnosed with vascular dementia. 2 years after surgery this very active jogger and weight lifter, golfer is in the late stages of Dementia! Is it the anesthesia and sedatives or is it oxygen deprivation during medical procedures??