Amyloid-ETA in 2024
Alzheimer’s is associated with toxic Amyloid-Beta proteins that form plaque in the brain. Nine years ago, researchers discovered another Alzheimer’s culprit called amyloid-ETA. Now in 2024, they’ve possibly figured out how it works.
Let’s first take a look at Amyloid-ETA. Then let’s see what’s new in 2024.
Where Does Amyloid Plaque Come From?

Chemical analysis of Alzheimer’s plaques reveals that they are made up of a family of short protein fragments, referred to as beta-amyloid peptides.
Beta-amyloid breaks off of a bigger protein called APP. The break is caused by the scissor-like action of two enzymes that “cut” an APP “thread” in two places. These two enzymes are called beta-secretase and gamma-secretase. Many clinical trials are trying to cure Alzheimer’s by stopping this series of events.
A New Cut

An international team of researchers led by Christian Haass (Professor of Metabolic Biochemistry at LMU and Speaker for the German Center for Neurodegenerative Diseases in Munich) and Dr. Michael Willem (LMU) made a discovery in 2015 which extends this picture of the pathogenesis of Alzheimer’s disease. This discovery has potentially far-reaching implications for our understanding of the condition:
“A second mode of APP cleavage exists, which involves a previously unknown cleavage and generates an alternative peptide,” says Christian Haass.
Eta
Its discoverers refer to the newly characterized protein fragment by the Greek letter eta, calling the protein “amyloid-eta” or ‘amyloid-η’.
“The processing pathway that produces it has been overlooked for 30 years. This is because investigators including myself have focused their attention on elucidating the origins of the beta-amyloid and on attempts to cure Alzheimer’s by inhibiting production of this peptide,” Haass explains. The paper that describes the generation of amyloid-η appears in the new issue of the journal “Nature”.
A Previously Unknown Interaction
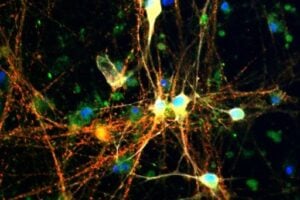
In collaboration with neurobiologist Dr. Hélène Marie based at the IPMC-CNRS in Valbonne (France) and with the local colleagues from the Technical University of Munich (TUM) in the Synergy Excellence Cluster (Professor Arthur Konnerth and Dr. Marc Aurel Busche), the LMU researchers have also studied the effects of the eta-amyloid on nerve-cell function in the brain. Beta-amyloid is known to make nerve cells hyperactive, and now it turns out that the eta-amyloid antagonizes this effect. “So here we have two small peptides snipped from the same precursor protein, which have opposite effects on neuronal activity, and whose actions must normally be carefully balanced,” Haass explains.
What This Means
These findings have immediate implications for the many ongoing clinical trials in humans targeted to beta-amyloid. One of the trials, for instance, is designed to ascertain whether or not pharmacological inhibition of beta-secretase (the enzyme that initiates the release of the toxic beta-amyloid from APP) can reduce memory loss in patients with Alzheimer’s. Haass, Willem and colleagues confirmed that blocking the action of the beta-secretase does indeed reduce levels of beta-amyloid. However, this is accompanied by a massive increase in the amount of eta-amyloid generated. “This could result in attenuation of neuronal activity and might therefore compromise brain function,” says Haass. He therefore suggests that investigators need to be on the look-out for any signs of unanticipated side-effects in the current clinical trials.
Amyloid-ETA Dampens Neural Activity
Thanks to this research, we now know that Amyloid-ETA dampens neural activity. But how? In 2024, after almost a decade of additional hard work and creative research, comes a possible answer. In the June 14 Neuron, the same researchers, led by Hélène Marie, Institut de Pharmacologie Moléculaire et Cellulaire, Valbonne, France, and Michael Willem at Ludwig-Maximillians-Universität, Munich, report that the peptides modulate NMDA glutamate receptors.
- Aη peptides modulate NMDA receptors and neural activity.
- They weaken long-term potentiation and strengthen long-term depression.
- Mice need them for their memory to function properly.
To really understand this in depth, a clear explanation and discussion, with complete diagrams, can be found on Alzforum, under the title, “Remember Amyloid-eta? A Decade Later, News on a Physiological Function“.
One thing is certain. The more we study Alzheimer’s, the more we get a sense of how complex it is and the multiple approaches we need to take in curing it. Discoveries like this have important implications on treating dementia today and beating Alzheimer’s in the not-too-distant future.










Continuing :Searching in Google with the title :"BRAIN STARVATION AS WE AGE APPEARS TO TRIGGER ALZHEIMER'S"
We can read about the work of professor Vassar as in the part of the text :"A study from the Feinberg School of Medicine has found when the brain doesn't get enough sugar glucose (or the . do Not gets enough energy) a process is launched that leads to Alzheimer's."
And, "A slow, chronic starvation of the brain as we age appears to be one of the major triggers of a biochemical process that causes some forms of Alzheimer's disease. A new study from Northwestern University's Feinberg School of Medicine has found when the brain doesn't get enough sugar glucose — as might occur when cardiovascular disease restricts the blood flow in arteries to the brain — a process is launched that ultimately produces the sticky clumps of protein that appear to be a cause of Alzheimer's. Robert Vassar, lead author, discovered a key brain protein is altered when the brain has a deficient supply of energy."
Professor Robert Vassar and colleagues (the researchers that discovered the BACE function) reported that in AD , "UPSTREAMS" , the VASCULAR AGEING, leads to the BRAIN ENERGY DEPRIVATION,by disorders in glucose transport and metabolization, and to mitochondrial disorders , etc.Then it Brain Energy Deprivation, that is responsible "DOWNSTREAMS", to INCREASES THE BACE1 LEVELS,increasing BETAMYLOID ACCUMULATION in the brains of the transgenic mouse model of AD.Then,using our Rational Thinking,if "UPSTREAMS",the Brain Energy Deprivation, leads to BACE accumulation , researchers could treat the brain energy deprivation, that in consequence will prevent and treat the BACE accumulation.If pharma companies,Instead to try to Search "DOWNSTREAMS",for BACE INHIBITORS,if they based in Vassar findings and in Logical Reasoning,starts to use and develops supplements (as ALCAR,Glucuronolactone,Carnosine,Ketones,etc.)and others drugs to Treat,"upstreams" the metabolical, molecular and biochemical disorders,that cause Brain Energy Deprivation,they will Increase the Brain Energy,Controlling in consequence the BACE Accumulation (and the betamyloid accumulation),in a more logical and "physiological" way, without No need of BACE INHIBITORS(and it aweful side effects).Just search in Google to the article in the site Alzheimer Research Forum, with the words:"Paper Alert: Energy Deprivation Drives Up BACE Translation"